Diabetic Retinopathy
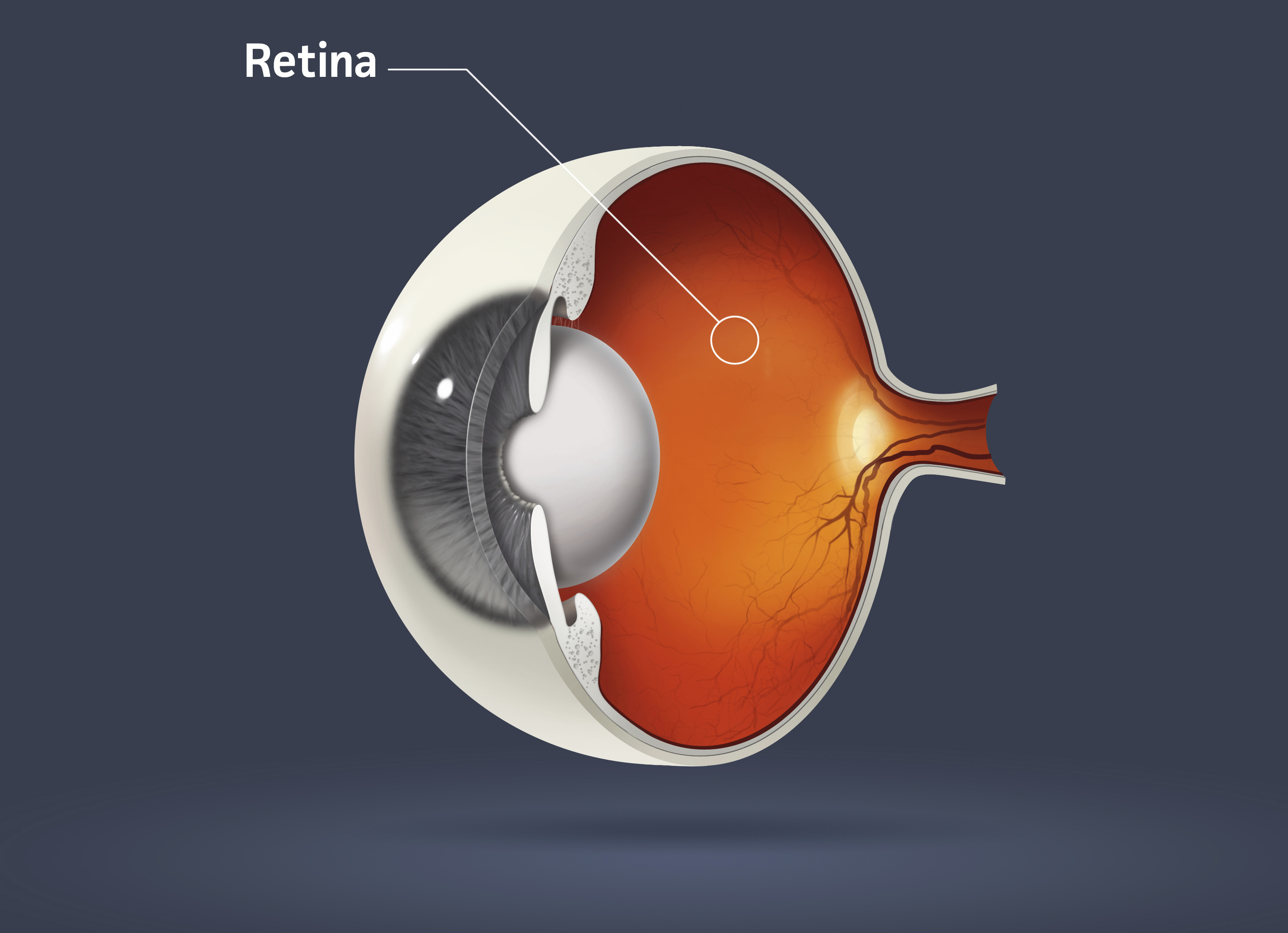
Diabetic retinopathy is a complication of diabetes that affects the eyes. It’s caused by damage to the blood vessels of the light-sensitive tissue at the back of the eye (retina).
At first, diabetic retinopathy may cause no symptoms or only mild vision problems. Eventually, however, diabetic retinopathy can result in blindness.
Diabetic retinopathy can develop in anyone who has type 1 diabetes or type 2 diabetes. The longer you have diabetes, and the less controlled your blood sugar is, the more likely you are to develop diabetic retinopathy.
To protect your vision, take prevention seriously. Start by carefully controlling your blood sugar level and scheduling yearly eye exams.
Too much sugar in your blood can damage the tiny blood vessels that nourish the retina. It may even block them completely. As more and more blood vessels become blocked, the blood supply to more of the retina is cutoff. This can result in vision loss. In response to the lack of blood supply, the eye attempts to grow new blood vessels. But, these new blood vessels don’t develop properly and can leak easily. Leaking blood vessels can cause a loss of vision. Scar tissue may also form, which can pull on the retina. Sometimes, this can cause the retina to detach.
Elevated blood sugar levels can also affect the eyes’ lenses. With high levels of sugar over long periods of time, the lenses can swell, providing another cause of blurred vision.
Symptoms
It’s possible to have diabetic retinopathy and not know it. In fact, it’s uncommon to have symptoms in the early stages of diabetic retinopathy.
As the condition progresses, diabetic retinopathy symptoms may include:
- Spots or dark strings floating in your vision (floaters)
- Blurred vision
- Fluctuating vision
- Dark or empty areas in your vision
- Vision loss
- Difficulty with color perception
Diabetic retinopathy usually affects both eyes.
Diabetic retinopathy may be classified as early or advanced, depending on your signs and symptoms.
- Early diabetic retinopathy. This type of diabetic retinopathy is called nonproliferative diabetic retinopathy (NPDR). It’s called that because at this point, new blood vessels aren’t growing (proliferating). NPDR can be described as mild, moderate or severe. When you have NPDR, the walls of the blood vessels in your retina weaken. Tiny bulges (called microaneurysms) protrude from the vessel walls, sometimes leaking or oozing fluid and blood into the retina. As the condition progresses, the smaller vessels may close and the larger retinal vessels may begin to dilate and become irregular in diameter. Nerve fibers in the retina may begin to swell. Sometimes the central part of the retina (macula) begins to swell, too. This is known as macular edema.
- Advanced diabetic retinopathy. Proliferative diabetic retinopathy (PDR) is the most severe type of diabetic retinopathy. It’s called proliferative because at this stage, new blood vessels begin to grow in the retina. These new blood vessels are abnormal. They may grow or leak into the clear, jelly-like substance that fills the center of your eye (vitreous). Eventually, scar tissue stimulated by the growth of new blood vessels may cause the retina to detach from the back of your eye. If the new blood vessels interfere with the normal flow of fluid out of the eye, pressure may build up in the eyeball, causing glaucoma. This can damage the nerve that carries images from your eye to your brain (optic nerve).
WHEN TO SEE A DOCTOR
Careful management of your diabetes is the best way to prevent vision loss. If you have diabetes, see your eye doctor for a yearly dilated eye exam — even if your vision seems fine — because it’s important to detect diabetic retinopathy in the early stages. If you become pregnant, your eye doctor may recommend additional eye exams throughout your pregnancy, because pregnancy can sometimes worsen diabetic retinopathy.
Contact your eye doctor right away if you experience sudden vision changes or your vision becomes blurry, spotty or hazy.
Diabetic retinopathy involves the abnormal growth of blood vessels in the retina. Complications can lead to serious vision problems:
- Vitreous hemorrhage. The new blood vessels may bleed into the clear, jelly-like substance that fills the center of your eye. If the amount of bleeding is small, you might see only a few dark spots or floaters. In more-severe cases, blood can fill the vitreous cavity and completely block your vision. Vitreous hemorrhage by itself usually doesn’t cause permanent vision loss. The blood often clears from the eye within a few weeks or months. Unless your retina is damaged, your vision may return to its previous clarity.
- Retinal detachment. The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. This may cause spots floating in your vision, flashes of light or severe vision loss.
- Glaucoma. New blood vessels may grow in the front part of your eye and interfere with the normal flow of fluid out of the eye, causing pressure in the eye to build up (glaucoma). This pressure can damage the nerve that carries images from your eye to your brain (optic nerve).
- Blindness. Eventually, diabetic retinopathy, glaucoma or both can lead to complete vision loss.
Treatment depends largely on the type of diabetic retinopathy you have. Your treatment will also be affected by how severe your retinopathy is, and how it has responded to previous treatments.
Early diabetic retinopathy
If you have nonproliferative diabetic retinopathy, you may not need treatment right away. However, your eye doctor will closely monitor your eyes to determine if you need treatment.
It may also be helpful to work with your primary care physician to find out if there are any additional steps you can take to improve your diabetes management. The good news is that when diabetic retinopathy is in the mild or moderate stage, good blood sugar control can usually slow the progression of diabetic retinopathy.
Advanced diabetic retinopathy
If you have proliferative diabetic retinopathy, you’ll need prompt surgical treatment. Sometimes surgery is also recommended for severe nonproliferative diabetic retinopathy. Depending on the specific problems with your retina, options may include:
- Focal laser treatment. This laser treatment, also known as photocoagulation, can stop or slow the leakage of blood and fluid in the eye. It’s done in your doctor’s office or eye clinic. During the procedure, leaks from abnormal blood vessels are treated with laser burns. Focal laser treatment is usually done in a single session. Your vision will be blurry for about a day after the procedure. Sometimes you will be aware of small spots in your visual field that are related to the laser treatment. These usually disappear within weeks. If you had blurred vision from swelling of the central macula before surgery, however, you may not recover completely normal vision. But, in some cases, vision does improve.
- Scatter laser treatment. This laser treatment, also known as panretinal photocoagulation, can shrink the abnormal blood vessels. It’s also done in your doctor’s office or eye clinic. During the procedure, the areas of the retina away from the macula are treated with scattered laser burns. The burns cause the abnormal new blood vessels to shrink and scar. Scatter laser treatment is usually done in two or more sessions. Your vision will be blurry for about a day after the procedure. Some loss of peripheral vision or night vision after the procedure is possible.
- Vitrectomy. This procedure can be used to remove blood from the middle of the eye (vitreous) as well as any scar tissue that’s tugging on the retina. It’s done in a surgery center or hospital using local or general anesthesia. During the procedure, the doctor makes a tiny incision in your eye. Scar tissue and blood in the eye are removed with delicate instruments and replaced with a salt solution, which helps maintain your eye’s normal shape. Sometimes a gas bubble must be placed in the cavity of the eye to help reattach the retina. If a gas bubble was placed in your eye, you may need to remain in a facedown position until the gas bubble dissipates — often several days. You’ll need to wear an eye patch and use medicated eye drops for a few days or weeks. Vitrectomy may be followed or accompanied by laser treatment.
Surgery often slows or stops the progression of diabetic retinopathy, but it’s not a cure. Because diabetes is a lifelong condition, future retinal damage and vision loss are possible. Even after treatment for diabetic retinopathy, you’ll need regular eye exams. At some point, additional treatment may be recommended.
Researchers are studying new treatments for diabetic retinopathy, including medications that may help prevent abnormal blood vessels from forming in the eye. Some of these medications are injected directly into the eye to treat existing swelling or abnormal blood vessels. These treatments appear promising, but they haven’t been studied in long-term trials yet.
